Haemorrhoids during pregnancy
8-minute read
Key facts
- Haemorrhoids (also known as ‘piles’) are swollen varicose veins located in the rectum and anus.
- Haemorrhoids are common in pregnancy.
- Haemorrhoids can cause symptoms including bleeding, pain or burning when you are doing a poo.
- If you have any symptoms of haemorrhoids, see your doctor, they can confirm a diagnosis and rule out more serious causes.
- The best way to treat and prevent haemorrhoids is by avoiding constipation, drinking plenty of water and eating a high-fibre diet.
What are haemorrhoids?
Haemorrhoids (also known as ‘piles’) are swollen varicose veins located in the rectum and anus (back passage). Haemorrhoids are common in pregnancy.
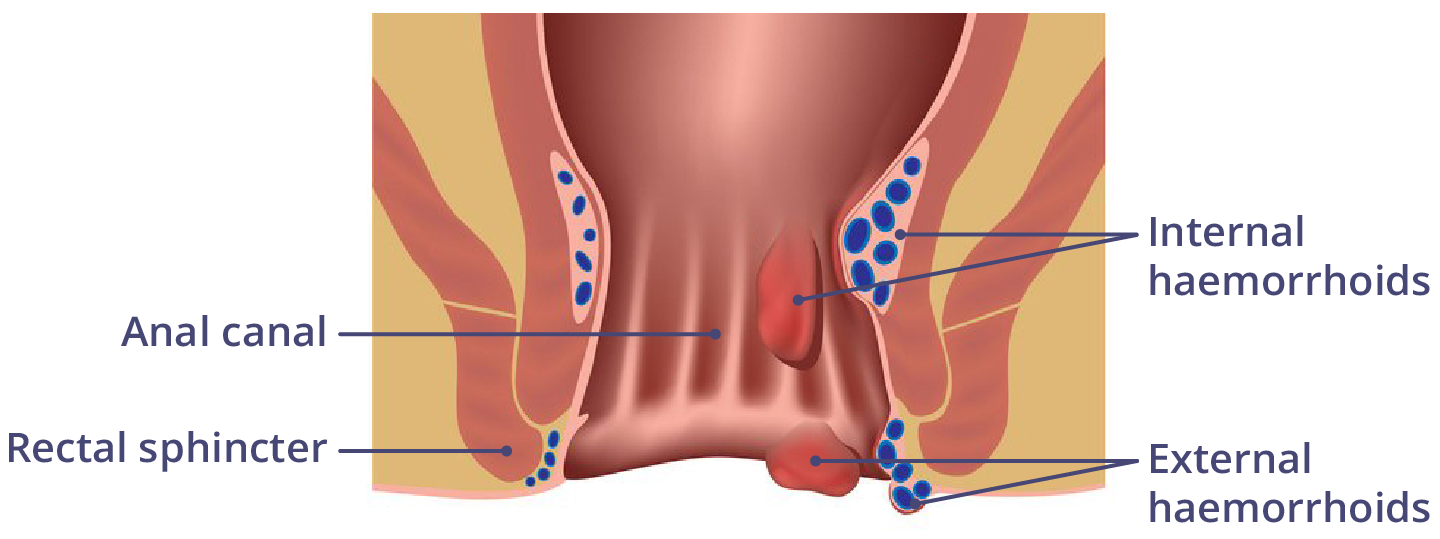
There are two main types of haemorrhoids:
- Internal haemorrhoids are not visible from the outside. Your doctor may see them while performing a visual or digital rectal examination (where the doctor examines your anus with a gloved finger).
- External haemorrhoids, where the veins swell and become visible from the outside.
Some people have both types of haemorrhoids at the same time.
What are the symptoms of haemorrhoids?
Haemorrhoids can cause symptoms including:
- bleeding from the rectum or anus
- pain or burning when doing a poo
- itching
External haemorrhoids are more likely to cause symptoms. Internal haemorrhoids generally don’t cause pain, but sometimes can cause minor bleeding.
CHECK YOUR SYMPTOMS — Use the Symptom Checker and find out if you need to seek medical help.
When should I see my doctor?
If you have pain when passing stools or see blood on the toilet paper or in your poo (stool), you should see your doctor. It might be the result of haemorrhoids, but it could be a sign of a more serious condition.
FIND A HEALTH SERVICE — The Service Finder can help you find doctors, pharmacies, hospitals and other health services.
What causes haemorrhoids during pregnancy?
During pregnancy, haemorrhoids can be caused by extra pressure on your rectal veins. This can happen from your uterus and pressure from your growing baby, and increased blood flow in the area.
Straining on the toilet because of constipation can also trigger or worsen haemorrhoids. Sometimes pregnancy can trigger symptoms from internal haemorrhoids, even if they previously did not cause symptoms.
When am I more likely to experience haemorrhoids during my pregnancy?
Pressure on the veins around your anus may get worse as your pregnancy progresses. This is due to your growing uterus and your baby’s increased size. For this reason, haemorrhoids are more common in the second and third trimesters of pregnancy.
Am I more likely to experience haemorrhoids if I had them before pregnancy?
If you know you had haemorrhoids before your pregnancy, take extra care, as they may get worse during pregnancy.
Not everyone with haemorrhoids has symptoms. If you first experience haemorrhoids during pregnancy, you might not be able to tell if this is new, or if you have had haemorrhoids in the past that did not cause symptoms.
ASK YOUR DOCTOR — Preparing for an appointment? Use the Question Builder for general tips on what to ask your GP or specialist.
How can I manage haemorrhoids during pregnancy?
During pregnancy, you can manage your haemorrhoids with simple treatment. They usually get better on their own after birth. Treatment options usually centre around preventing or managing constipation and reducing associated pain.
Treatment options include the following:
- Lifestyle changes — a diet high in fibre and drinking lots of water will help ensure you don’t need to strain on the toilet. External haemorrhoids can be treated by placing an icepack on the affected area to reduce swelling. Taking a warm bath may also help to reduce the pain.
- Laxatives — help ease any straining associated with constipation. They help you pass bowel movements (poo) more easily.
- Pain relief medicines — paracetamol can help reduce pain associated with sore, swollen veins, and can be taken during pregnancy. Make sure to follow the directions for use.
- Haemorrhoid creams — help reduce itchiness, pain or inflammation, and contain active ingredients such as corticosteroids or local anaesthetics.
Check with your doctor or pharmacist before using medicines or creams while pregnant.
Could haemorrhoids be a sign of something more serious?
If you think you might have haemorrhoids, it is important to tell your doctor.
This is because symptoms such as bleeding from your bowel or anus can be a sign of more serious conditions.
Will haemorrhoids affect my baby?
Haemorrhoids in pregnancy will not affect your baby. They can be uncomfortable for you and may need treatment, but there are safe ways to help manage the symptoms of haemorrhoids while you are pregnant.
There is some concern that the pushing stage of labour and birth can worsen your haemorrhoids. Speak to your midwife if you are concerned about haemorrhoids during your pregnancy or birth.
Will haemorrhoids continue after I’ve had my baby?
In most cases, haemorrhoids go away within a few days after your baby is born.
If you find your haemorrhoids do not get better after giving birth, speak to your doctor or pharmacist about treatment.
Can haemorrhoids be prevented?
Avoiding constipation is the best way to reduce your chance of haemorrhoids. A healthy gut will prevent the need to strain when you are doing a poo. You should also:
- eat a diet high in fruit, vegetables and wholegrains
- drink plenty of water
Resources and support
If you have more questions about haemorrhoids during your pregnancy, you can consult with:
- your doctor or midwife
- a pharmacist
- an obstetrician
- an accredited dietitian
Visit NSW Health to read more about haemorrhoids in pregnancy and breastfeeding.
Read the fact sheet on lesser-known pregnancy symptoms, at the Gidget Foundation.
Download the Monash Women’s Health booklet Your pregnancy – what to expect and what you can do.

Speak to a maternal child health nurse
Call Pregnancy, Birth and Baby to speak to a maternal child health nurse on 1800 882 436 or video call. Available 7am to midnight (AET), 7 days a week.
Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: February 2025



