Blocked tear ducts in babies
7-minute read
Key facts
- A blocked tear duct is also known as 'sticky eye'.
- A blocked tear duct is not an infection and should not cause your child pain.
- This condition usually gets better by itself, but it's still wise to check with your doctor.
- There are things you can do to help sticky eye get better and avoid infection.
What is a blocked tear duct?
A blocked tear duct in babies is also known as 'sticky eye'. The term sticky eye can also be used for conjunctivitis, which is an eye infection.
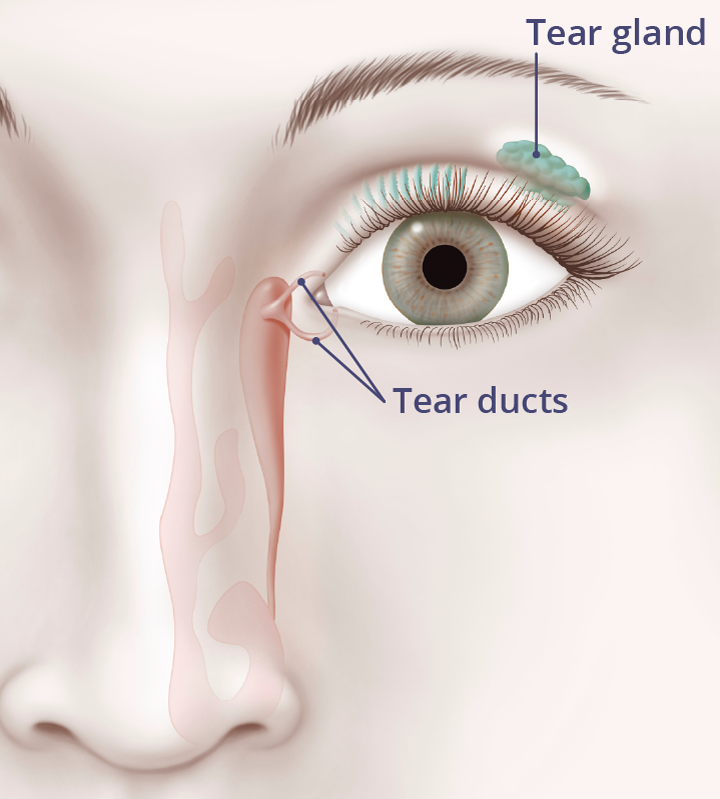
Tears normally drain away through small openings in the inside corner of your eyelids. They enter the nose through the nasolacrimal ducts (tear ducts).
Sometimes, when babies are born, their tear ducts have not yet opened normally. This can cause watery or sticky eyes.
What are the symptoms of a blocked tear duct?
If your baby has a blocked tear duct their eye or eyes will water a lot. They may have tears running down their cheeks. Sometimes there may be swelling or a sticky discharge.
Having a blocked tear duct is not an infection and should not cause your child pain.
CHECK YOUR SYMPTOMS — Use the Symptom Checker and find out if you need to seek medical help.
What causes a blocked tear duct?
A blocked tear duct usually happens because the thin layer (membrane) at the end of the tear duct doesn’t open normally at birth.
As many as 1 in every 20 babies has blocked tear ducts. This may be unilateral (one eye only) or bilateral (both eyes).
This means their tears can't drain away and their eyes are wet all the time.
When should I see my doctor?
You should always see your doctor if you think your baby has an eye infection.
You should also see your doctor if:
- your baby seems sensitive to light
- they have large amounts of eye discharge
- they are constantly squeezing their eyes shut
- the side of their nose seems swollen, red, and painful
- the white part of their eye is red or blood shot
- the tear duct is still blocked by the time they reach 1 year of age
FIND A HEALTH SERVICE — The Service Finder can help you find doctors, pharmacies, hospitals and other health services.
How is a blocked tear duct treated?
In 9 out of 10 babies born with blocked tear ducts, their tear ducts will open on their own by the time they are 1 year old.
Some babies will need surgery if their blocked tear duct doesn't improve. This is done as day surgery with a general anaesthetic. Your doctor may treat a blocked tear duct in these ways:
- Open the tear duct and flush it out.
- Use a silicone tube to keep the duct open — this will be left for a few months to make sure that the blockage doesn't happen again.
- Make a new opening between the tear sac and the bone in the nose (dacryocystorhinostomy).
How do I manage my baby's blocked tear duct at home?
It's a good idea to clean your baby's eyelids and gently massage their tear duct. This can stop infections and help the tear duct to open.
Your doctor or child health nurse can show you how to clean your baby’s eye and how to massage the tear duct.
What are the complications of a blocked tear duct?
A blocked tear duct is not an infection, but it can put your baby’s eye at risk of developing an infection.
Conjunctivitis
Conjunctivitis is an eye inflammation caused by an infection or allergy.
It can be difficult to tell the difference between the symptoms of a blocked tear duct and conjunctivitis.
If you think your baby may have conjunctivitis, see your doctor as soon as you can, so your baby can start treatment.
Dacryocystitis
If your baby’s tear duct becomes infected you will see a firm, red, painful lump at the side of their nose. There may also be yellow-green discharge. This is called dacryocystitis.
If this happens, you should call your doctor or ophthalmologist urgently. Your baby will need antibiotics to treat the infection.
Resources and support
Talk to your doctor or child health nurse if you have questions about blocked tear ducts in babies.
Read more about blocked tear ducts at healthdirect.

Speak to a maternal child health nurse
Call Pregnancy, Birth and Baby to speak to a maternal child health nurse on 1800 882 436 or video call. Available 7am to midnight (AET), 7 days a week.
Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: July 2025



